
Divisions
- Community Partnerships and Priorities
- Digital Strategy and Services
- Office of Local Government
- Office of Parliamentary Counsel
- Office of Review and Evaluation
- Office of the Secretary
- Resilience and Recovery Tasmania
- Corporate and Government Services
- Policy Division
- Service Tasmania Unit
- State Service Management Office
Contact Details
By phone
Find the number of a specific division or office to contact them directly or call Service Tasmania on 1300 135 513.
Our staff
Use the Tasmanian Government Directory to find staff contact details
Social media
Follow our social media accounts to keep up to date with specific programs and initiatives.
1. Public health and health system preparedness for the outbreak
1. Public health and health system preparedness for the outbreak
Despite significant challenges associated with managing and responding to the pandemic in the context of the progress of the pandemic internationally, Tasmania’s public health and health system preparedness was supported by the state’s existing frameworks, established forums, and protocols specifically designed to be rapidly activated during an emergency.
These include:
- existing emergency management frameworks and coordination arrangements (including established pandemic response plans);
- associated legislative frameworks (including statutory powers held by the Director of Public Health (DPH));
- pre-existing emergency management structures, such as the State Emergency Management Committee (SEMC), and the State Health and Human Services Emergency Committee;
- operational systems and processes, including both existing systems (such as established procurement and supply arrangements) and those implemented in direct response to the virus (for example those established to ensure safe assessment and testing capacity across the state); and
- engagement in relevant national forums to inform and support Tasmania’s pandemic response.
Tasmania’s response to the pandemic was initially guided by pre-existing state and national planning for Pandemic Influenza (given the relevancy and applicability of the approaches and activities in that planning) and subsequently by dedicated COVID-19 response plans that were developed and updated in line with new and emerging information on the virus.
A key component of the DoH’s planning included taking steps to ensure Tasmania’s public hospitals were appropriately resourced to provide safe care for patients during the pandemic (for both those with and those without COVID-19 infection). Consistent with the lessons emerging from the experience of countries such as Italy, proactive steps were taken early in the pandemic to ensure maximised public hospital capacity. This included restricting elective surgery across the public and private sectors, surge capacity planning, and measures to ensure availability of critical medical equipment and resources as outlined further under this section (with detailed information regarding management of personal protective equipment (PPE) provided under section 4).
1.1 Emergency management framework
Tasmania’s existing emergency management framework supported early health system preparedness and responses.
The State Special Emergency Management Plan (SSEMP): Pandemic Influenza 2019 (SSEMP: PI) outlines health and whole-of-government arrangements including management authority, escalation triggers and responses, and cross-agency responsibilities. While designed to respond to predictable influenza outbreaks, this plan was adapted and used by the DoH to guide Tasmania’s response to the pandemic, prior to the development of the COVID-19 specific SSEMP (SSEMP: COVID-19).
The SSEMP: COVID-19 was rapidly developed by the DoH (based on the SSEMP: PI) and formally approved by the State Controller on 17 March 2020. The SSEMP: PI and subsequently the SSEMP: COVID-19 have been used alongside other state and national response planning documents and processes to inform Tasmania’s health system response to the pandemic.
The existing Interoperability Arrangements for Sharing Skilled Resources in Tasmania (the Interoperability Arrangements) were also utilised. The Interoperability Arrangements are standing emergency management arrangements allowing for sharing of staff between Tasmanian Government agencies during an emergency. These arrangements have been crucial throughout the pandemic and during the outbreak, allowing staff to be quickly redirected from across a range of government agencies to support management of the outbreak.
1.2 COVID-19 emergency management response levels and escalations
Through application of established health emergency management escalation frameworks, including the SSEMP: PI and SSEMP: COVID-19, the DoH’s pandemic response efforts were able to be coordinated and escalated in response to the emerging and increasing threat presented by the virus. These measures were critical to management of the North West outbreak itself, enabling the rapid escalation of the response at the NWRH in line with the increase in cases in the North West.
It should be noted that in the early weeks of the emerging virus threat, there was little talk of elimination. Tasmania’s approach, as with the rest of Australia, was to maintain infection, hospitalisation and critically ill case numbers low for long enough in order to build the necessary capacity in the system to face what was being predicted to be a significant surge in morbidity and mortality. This was to be through the development of workforce, consumable and infrastructural capacity to ensure the provision of care that would best protect patients, staff and the community. This was the approach of “flattening the curve”- recognising that while infection numbers may still be high, they could be delayed for long enough to enable the development of greater response capacity.
Further detail on how the health emergency management response levels were activated is outlined below.
1.2.1 Level 1 response
In late January 2020, the DoH stepped up to a Level 1 health emergency management response (the SSEMP: COVID-19 sets out the response levels). This was prior to the declaration by the WHO of the COVID-19 outbreak as a public health emergency of international concern on 30 January 2020, and subsequently as a pandemic on 11 March 2020.
An Incident Management Team (IMT) was established within the DoH’s PHS in late January 2020, led by the DPH as Incident Controller and supported by the Tasmanian Chief Medical Officer (CMO). Through the IMT, DoH worked closely with national contacts to ensure a consistent approach to assessment, testing, care and advice for healthcare workers, other government agencies and the public.
From early February 2020, the IMT included representation from Primary Health Tasmania and the THS to ensure timely information and updates were provided to local general practitioners (GPs), hospitals and other sectors (to ensure healthcare workers were aware of protocols in place to identify and manage confirmed and suspected COVID-19 cases).
An interdepartmental committee (IDC) was also established to enable cross-agency coordination of response efforts. The SEMC, chaired by the State Controller (Commissioner of Police) and with the DoH as the SEMC Advisory Agency, was subsequently stood up (as announced on 28 February 2020) to lead the whole-of-government coordination of the COVID-19 response in Tasmania, taking on from the IDC the function of providing cross-agency oversight.
1.2.2 Level 2 response
On 5 March 2020, the DoH Secretary approved escalation to Level 2 health emergency management response under the SSEMP: COVID-19. The decision to escalate was made due to a number of factors including (but not limited to):
- systems pressure (including the potential for a confirmed COVID-19 case in Tasmania driving a rapid rise in presentations to primary and acute health services);
- increasing demand for specimen collection and testing, disease surveillance and clinical treatment;
- whole-of-government impacts (requiring increased liaison and intergovernmental relations); and
- growing potential for fatigue of the workforce supporting the response (with growing need for a long-term strategic, system-level COVID-19 response).
Under Level 2 the DoH Secretary established the DoH Emergency Coordination Centre (ECC), and appointed an Incident Controller to lead the ECC, enabling the DPH to be appropriately focussed on continuing to lead the public health response, providing advice to government, and liaising and collaborating with national counterparts.
The ECC is responsible for system-wide consequence management, including the strategic leadership, coordination and direction of system-wide and service level COVID-19 preparedness and response activities and consequence management arrangements. The ECC draws on the specialist advice of all departmental areas and service groups to manage and coordinate the rapidly increasing demand on the health system. Establishment of the ECC ensured there was one dedicated team focussed on the management of the Tasmanian health system response, staffed by people from across the DoH and beyond with specific expertise in key areas including logistics and resourcing, communications, health systems operation and service delivery, and heath emergency planning and policy. Critically, timely establishment of the ECC also ensured operational/service groups were not avoidably diverted from continuing to provide the DoH’s core business functions.
Key functions of the ECC in the COVID-19 response have included (but are not limited to):
- monitoring the strategic condition of the DoH COVID-19 response operations and consequence management;
- establishing and maintaining liaison with key stakeholders at the intra/inter-agency and intergovernmental level;
- managing and distributing situation information (further detail on communication/information sharing mechanisms and processes is provided under section 3 below);
- facilitating and coordinating requests for information and/or assistance from and between the Australian Government and other states and territories (related to the health system response);
- monitoring supply levels (for resources such as PPE, ventilators, pharmaceuticals, testing swabs and reagents, and other medical consumables, identifying alternate supply sources/mechanisms, and ensuring the quality of obtained resources;
- procuring resources to ensure increasing demand is met (for example raising requests for resources from the National Medical Stockpile. The National Medical Stockpile, which is administered centrally by the Australian Government and controlled locally by the Tasmanian CMO, is a strategic reserve of resources such as medications, vaccines and PPE for use in national health emergencies;
- intra-jurisdictional coordination, ensuring resources were directed to areas where there was greatest need (while also ensuring availability of stock statewide to address current needs and potential further outbreaks); and
- monitoring and addressing staffing and other logistics issues (including through use of the Interoperability Arrangements to support and bolster the workforce dedicated to the COVID-19 response).
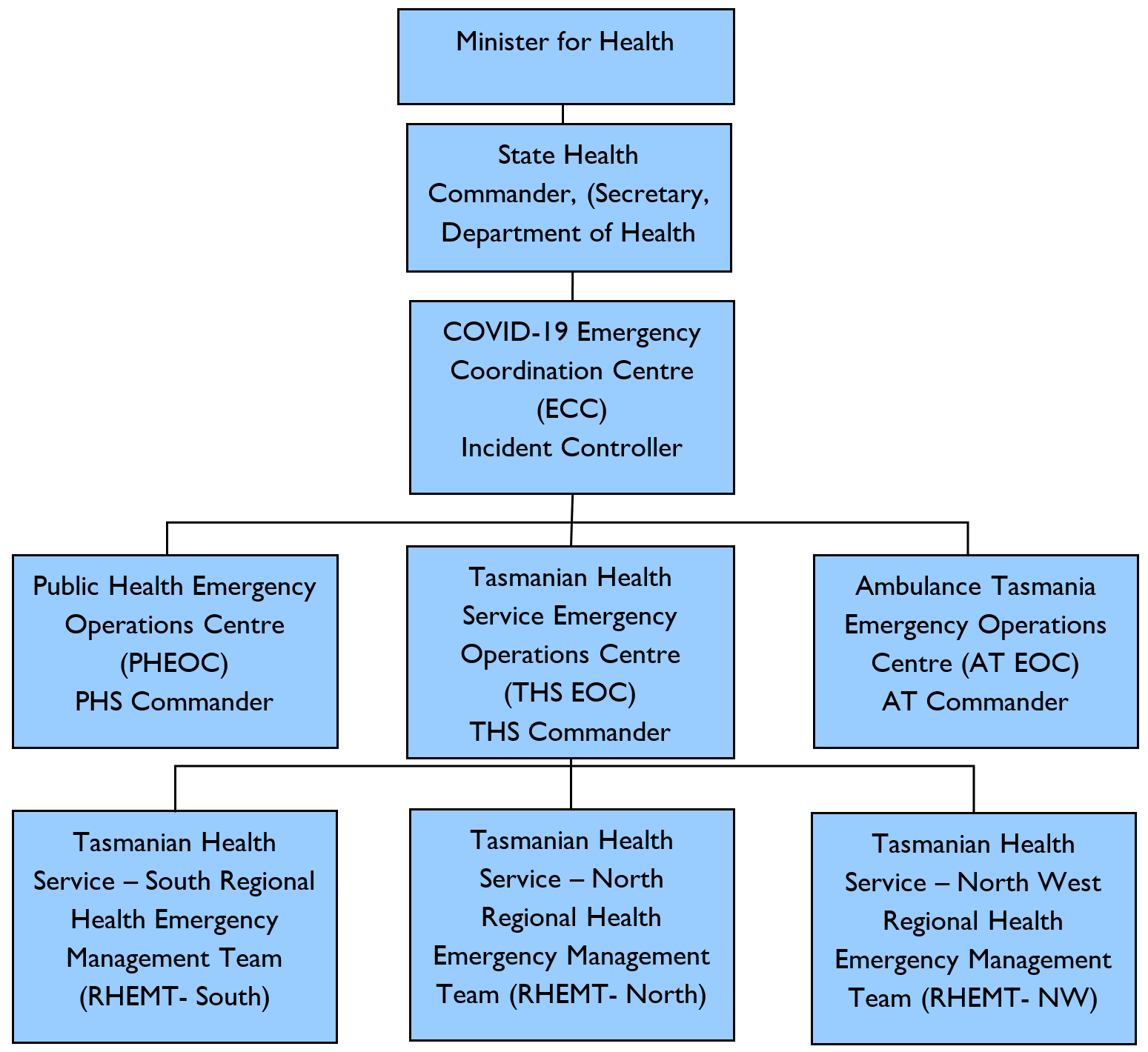
The ECC has been supported by three emergency operations centres (EOC) also activated under the Level 2 response, the Public Health EOC (PHEOC), the THS EOC, and the ATEOC. Each EOC, led by an EOC Commander, provides specific, specialised operational advice to the ECC and is responsible for the coordination and management of COVID-19 response operations and consequence management in their service areas. Access to timely operational advice, including the ability to direct, manage and coordinate response operations at the individual service level, was a key factor in enabling rapid responses to emerging issues throughout the pandemic response.
Under the Level 2 response, three Regional Health Emergency Management Teams (RHEMTs) were also activated to support the THS EOC. The RHEMTs play a key role in managing and coordinating THS regional level emergency response operations, with direction provided through the THSEOC Commander. Each RHEMT is led by a Regional Health Commander. The RHEMTs report to the ECC via the THS EOC.
Each RHEMT, with membership drawn from broad representation across the THS and liaising closely with key stakeholders (such as primary health, private providers, AT and others), is responsible for maintaining local lines of communication, providing advice through the THS EOC to the ECC, clarifying issues of policy or implementation, and ensuring local escalation plans are developed for endorsement by the ECC and State Health Commander.
The Level 2 emergency management structure is set out in Figure 1.
Figure 1: Level 2 Emergency Management Structure
Under Level 2, the Secretary DoH formally assumed the role of State Health Commander, providing oversight and direction to the Incident Controller, and briefing the Minister for Health and the Ministerial Committee on Emergency Management of Cabinet as required regarding the health system response and emerging issues.
On 17 March 2020, the DPH declared a Public Health Emergency under Section 14 of the Public Health Act 1997 (Tas) (the Public Health Act). This allowed the DPH to use a suite of emergency powers under the Public Health Act to support Tasmania’s pandemic response. These powers were utilised both during the North West outbreak and broader statewide responses (discussed further below and under Section 2 of this submission).
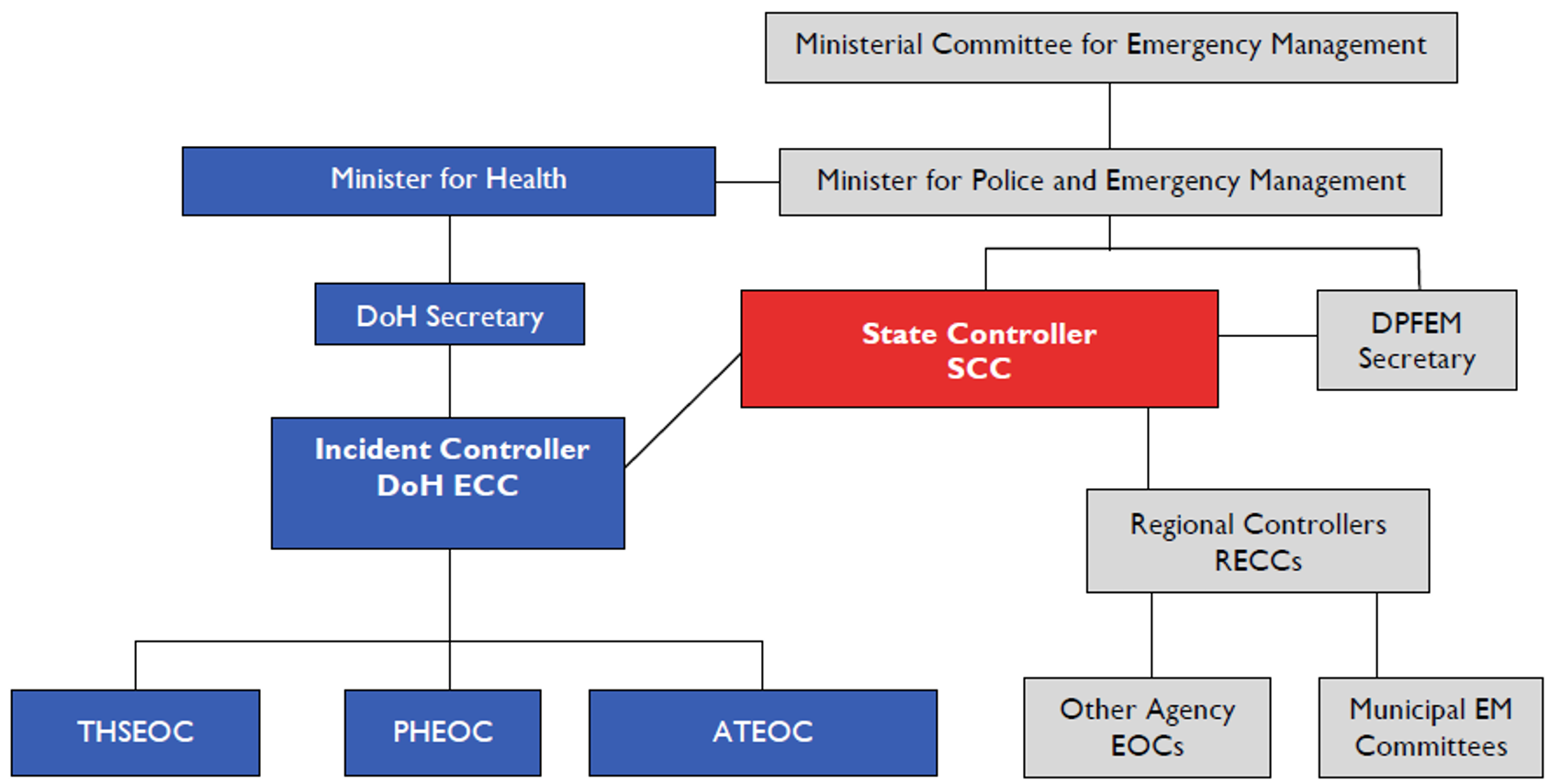
1.2.3 Level 3 response
On 19 March 2020, the Premier declared a State of Emergency, with the State Controller approving escalation to a Level 3 emergency management response under the SSEMP: COVID-19. Under the Level 3 response the State Control Centre (SCC) was activated to lead coordination of the whole-of-government response to the pandemic, led by the State Controller in close liaison with the State Health Commander, the Incident Controller, the DPH and the CMO. Powers available to the State Controller under the Emergency Management Act 2006 (Tas) (the Emergency Management Act) were used to support the North West outbreak response (as described under Section 2 of this submission). Under Level 3, the DoH has continued to coordinate the health sector response through the structures established and activated under the Level 2 response.
The Level 3 emergency management structure is set out in Figure 2 below.
Figure 2: Level 3 Emergency Management Structure
1.3 Legislative framework
As set out under the SSEMP: COVID-19, Tasmania’s response to COVID-19 has been supported by an existing legal framework including powers available under the Emergency Management Act and Public Health Act. Under the Public Health Act, the DPH has used a wide range of standing and emergency powers to respond to, and minimise, the impacts of the North West outbreak (discussed further under Section 2 of this submission), and in Tasmania’s broader pandemic preparedness and response efforts.
Directions issued by the DPH in the earlier stages of the pandemic response (prior to the North West outbreak) were targeted at preventing virus spread, and included directions regarding:
- restrictions on gathering size;
- restrictions on operations of certain premises;
- requirements for social distancing;
- isolation and quarantine requirements;
- restrictions on visitors to aged care facilities; and
- restrictions on movement of people from their primary residence (stay at home).
Directions issued by the DPH throughout Tasmania’s pandemic response have been informed by the current national guidance at the time of issue of each Direction (including statements issued by the Australian Health Protection Principal Committee (AHPPC), Communicable Disease Network Australia COVID-19 Series of National Guidelines for Public Health Units (the CDNA SoNG) and decisions published by National Cabinet, with consideration also given to specific local context where required (for example consideration of current virus prevalence and likely risk of spread).
1.4 Availability of assessment and testing services
Ensuring the availability of early, accessible and safe assessment and testing for COVID-19 aligned with national guidance, has been a vital component of state and national efforts to flatten the curve. An example of this was the early establishment of respiratory clinics by both the Tasmanian and Australian Governments. Through the health emergency management structure detailed above, the DoH has been able to monitor both demand and capacity for testing across the state, provide relevant guidance to operational areas (such as updates to testing criteria), and progress measures as outlined below to ensure demand for testing has been continually met.
National guidance regarding testing processes and criteria for testing has evolved in response to new information on the epidemiological characteristics of the virus (including the prevalence and potential for spread), clinical case definition, and testing capacity. Tasmania’s COVID-19 testing policies and processes have in turn evolved throughout the pandemic response in line with national guidelines and recommendations set out in the CDNA SoNG.
In early March 2020, in line with the SSEMP, and under the Level 2 response, DoH established and commenced operation of four testing clinics across the state to provide safe dedicated facilities for the assessment and testing of people with respiratory symptoms. These facilities were established to minimise the risk of transmission of COVID-19 in other health care settings, such as general practice, hospital emergency departments and outpatient clinics, and to reduce pressure on public hospitals caused by increased respiratory presentations. These state-run clinics were complemented by four GP-led respiratory clinics funded by the Australian Government (coordinated by Primary Health Tasmania).
Additional mobile and demountable clinics were also purchased and fitted out by the DoH in preparation for anticipated increases in presentation of people with respiratory illness or symptoms (both due to COVID-19 and influenza). These include four buses fitted out and utilised as mobile clinics, and the purchase of modular clinics to be installed at three locations across the state (with capacity for eight consultation rooms at each location). The mobile clinics were used during the North West outbreak to enable the safe provision of vital assessment and testing services.
The DoH has sourced testing supplies through a range of suppliers and from the Australian Government National Medical Stockpile. Reagent and supplies were monitored (and the majority ordered) internally by the Royal Hobart Hospital (RHH) Laboratory with reports on current supply levels and supply issues provided to the ECC. Securing and maintaining adequate testing supplies has been an ongoing challenge of concern across Australian jurisdictions and internationally. To date, Tasmania has been able to procure and retain enough stock of testing supplies to meet demand for testing throughout the pandemic, including the increased demand for testing both the community and staff members during the North West outbreak. In addition to testing consumables, the capacity of the RHH Molecular Laboratory has also been significantly expanded to cater for testing surge capacity; with the purchase and commissioning of additional Polymerase Chain Reaction (PCR) equipment and the move into a larger refitted laboratory, capacity for testing has increased to approximately 2 000 tests a day. Private laboratory capacity has also improved, with the installation of private PCR capability in June 2020, with capacity to undertake approximately 200 tests a day. This has subsequently increased to approximately 500 tests a day in August 2020.
1.5 Engagement in national committees
The Tasmanian Government has worked closely with the Australian Government throughout the pandemic.
The DoH has engaged closely with the chief executives and clinical and public health leads of the Australian Government Department of Health and all state and territory health departments in the lead up to, and throughout, the pandemic. This has ensured Tasmania’s health system response has aligned (where possible and appropriate) with current agreed national approaches and guidance.
Through the DPH’s participation in daily AHPPC meetings and out‑of-session consideration of issues, DoH representation on related committees such as the CDNA, and the DoH Secretary’s engagement with Australian Health Ministers’ Advisory Council, the DoH has contributed to the development of national COVID-19 response planning, policies and recommendations. This has included input on the development of and revisions to testing criteria, contact tracing, scope of restrictions (i.e. those put in place through Directions issued by the DPH) and social (or physical) distancing requirements, elective surgery restrictions, and distribution of medical supplies and equipment.
In addition to officer level engagement, Tasmania's Minister for Health has participated in regular meetings with other State and Territory Health ministers, and the Australian Government Minister for Health, as well as the Australian Government Chief Medical Officer. This process enabled regular updates on Australian Government assistance to the State, as well as briefing on emerging issues. Through these national engagement mechanisms, Tasmania’s interests have been represented in consideration of the national health response and contributed to advice to inform National Cabinet discussions. It is important to note that the need for timely and rapid health system response has meant that Tasmania has progressed interim measures and solutions while national approaches were being developed and finalised (for example to secure PPE supplies) to ensure that Tasmania was adequately resourced to manage increased presentation and spread of the virus.
In March 2020, Tasmania, along with all other states and territories, negotiated the COVID-19 National Partnership Agreement (the COVID-19 NPA). Under the COVID-19 NPA, the Australian Government provides financial assistance for additional costs incurred by state and territory health services in responding to the COVID-19 outbreak, including as a result of the diagnosis and treatment of patients with, or suspected of having, COVID-19, and efforts to minimise the spread of COVID-19. The COVID-19 NPA commenced on 13 March 2020. It was subsequently amended in early April 2020 to include the Australian Government’s financial viability payment for private hospitals, which ensured private hospitals committed to retain capacity to assist states to respond to COVID-19.
1.6 Infection Prevention and Control Training
THS medical, nursing and allied health professionals are trained in infection prevention and control practices. Annual participation in PPE use and hand hygiene education is mandatory for these professional groups. Leading up to and throughout the pandemic the THS has worked to ensure staff are aware of current national guidance regarding the use of PPE and broader infection control. This has included online training resources on PPE use (discussed in detail under Section 4 of this submission) and implementation of appropriate infection control management strategies to minimise transmission within the health care setting.
Areas of Tasmania’s major hospitals also ran a series of internal scenario-based simulation training exercises as part of overall preparedness for COVID-19. These COVID-19 specific simulations were incorporated into established training programs, with a range of intradepartmental exercises taking place to support organisational preparedness.
At the RHH, various Departments undertook a range of scenario training covering receiving and transferring COVID positive patients, responding to deteriorating patients and the use of PPE. COVID-19 specific training sessions commenced in early March 2020 to help prepare staff and also focused on communicating with patients and families.
The Launceston General Hospital (LGH) commenced simulation training in mid-February 2020. This included Critical Care Simulation Training covering donning and doffing of PPE, transfer of patients and the role of spotters and clean teams for staff across multiple departments. Upskilling of staff to increase the number of staff capable of providing care to critical care/high dependency patients was also undertaken.
In the North West there was regular communication with managers and staff relating to training, resources and protocols for the management of COVID-19 including:
- PPE training resources circulated to staff from late January 2020.
- Infection control training for cleaning staff in early February 2020.
- Training from late February and throughout March 2020 for medical and surgical staff, hospital auxiliary, attendants, catering, theatre, anaesthetics, emergency department/ambulance and speech therapy and pharmacy staff covering issues such as hand hygiene, social distancing, and respiratory hygiene and cough etiquette.
- Clinical staff orientation on COVID-19 respiratory screening, including (in addition to PPE training) specimen collection and documentation training in March 2020
- COVID-19 intubation training for anaesthetic and emergency department clinicians in March 2020.
All AT operational staff are highly trained in PPE use and broader infection prevention and control practices. AT staff regularly participate in mandatory training to ensure their practices are in line with current national requirements and best practice guidance.
In addition to providing mandatory training in PPE use for all staff and volunteer ambulance officers (commencing in March 2020), AT also undertook further COVID-19 preparedness training, including:
- “just in time” training which focused on preparing appropriately experienced AT staff for a potential field hospital scenario (as demonstrated in other countries), with a focus on enhancing intensive care unit (ICU) capacity;
- enhanced PPE training for the transport of highly or potentially highly infectious patients; and
- ongoing provision of updated guidance to AT staff regarding internal processes and protocols, and state and national guidance for the management of patients suspected or confirmed as being COVID-19 positive.
In additional to infection prevention, contact tracing and case management are core business of PHS with respect to disease outbreak management. PHS performs these functions across a broad range of communicable diseases as part of its business as usual activity. As such, additional training for PHS staff regarding these activities was not required in preparedness for the pandemic. However, during March, support from other business units necessitated training for new people coming in to assist and this occurred. At later stages (following commencement of the North West outbreak) PHS enhanced information and training capability to skill-up a surge workforce to respond to the growth in numbers and consequent demand for contact tracing and case management.
1.7 Hospital-level planning, including Intensive Care Unit surge and staffing capacity
Early in the pandemic a key focus of preparation was hospital and ICU surge capacity planning. This was largely driven by the prevailing international experience in countries such as Italy, where extreme pressure was experienced in their hospital systems as cases of COVID-19 surged. Thankfully, the NWRH outbreak ultimately did not result in extreme demand for hospital and ICU resources, but this early planning has ensured Tasmania’s hospitals are well placed to respond to any future COVID-19 outbreak. The plans put in place in March and early April 2020 to provide a framework for escalation, and the capacity to draw upon statewide hospital resources once the NWRH and the North West Private Hospital (NWPH) were closed, proved to be important components of managing the NWRH outbreak. These are outlined in greater detail in Section 2 below.
During March 2020, each of Tasmania’s four major public hospitals were developing plans and strategies to ensure essential hospital services could continue to be delivered while minimising the risk of transmission of COVID-19 to patients and staff.
Ongoing monitoring of stock and medical equipment (including ventilators, medications and PPE) commenced in March 2020 in preparation for a potential surge in demand. Further information on this specific planning is outlined below. Planning was also undertaken to identify additional beds across the state’s public hospitals that might be used to increase surge capacity, including identification of additional ICU beds and beds that could be readily converted to provide care for ventilated patients if required.
Through the DoH’s strong established relationships with private providers in Tasmania, the THS also progressed early planning with regional private hospitals to support and increase public hospital capacity in the event of a surge in demand. The key purpose of these arrangements was to free up public hospital beds to respond to a potential increase in COVID-19 cases, and was closely tied with national restrictions on elective surgery.
Hospitals also commenced planning aimed at ensuring a suitably trained workforce was available to operationalise an increase in beds. This planning included a focus on identifying appropriately trained health care workers to staff increased ICU beds in the event of a surge in critically unwell or ventilated patients.
Hospitals were also reconfigured to allow for triaging and treatment of patients with COVID-19 while limiting their exposure to other patients. The public hospital emergency departments were repurposed so as to provide separate areas for the care of those presenting with acute respiratory illness, in whom COVID‑19 infection could not be excluded. This meant that the assessment and treatment of people presenting with severe symptoms consistent with possible COVID-19 infection could be undertaken in dedicated areas with staff undertaking additional precautions. Dedicated isolation wards were also established in each hospital with the aim of reducing the risk of transmission of COVID-19 from a hospitalised case.
In early April 2020, Escalation Management Plans were approved for each of the three THS regions (South, North and North West). These initial plans were the operational documents outlining the THS response arrangements for COVID-19, including alignment (where appropriate) with agreed national and health sector arrangements. The plans detail a four-tier escalation response with clear trigger points for each level, which became an important guiding factor for decision-making during the NWRH outbreak, as outlined in Section 2 below. The Plans also outlined statewide surge capacity in the event of an escalation in COVID-19 patients, including the utilisation of resources across the state to assist in meeting localised increases in demand.
Plans were developed through a collaborative approach. For example, in the NW the detail for inclusion in the NW Escalation Management Plans was through local unit level and facility level action plans. A range of consultation was undertaken with the clinical directors, nursing unit managers and/or department heads of each area including sign off for the level at which the triggers were set and the actions were to be taken.
In addition to the THS Escalation Management Plans, the THS also developed a range of other plans including:
- THS District Hospital Escalation Management Plans (South, North, North West) to outline the response and recovery arrangements for the district hospitals.
- THS Intensive Care Unit (ICU) Surge Capacity Plan to outline the actions and duties to be taken by the Tasmanian Critical Care Network in response to COVID-19. The ICU Surge Plan is read in conjunction with the THS Escalation Management Plans.
1.8 Availability of medical resources including ventilators, medical consumables and pharmaceutical supplies
As part of regular business, supply of medical equipment for Tasmanian public hospitals, including PPE, has been centrally managed by the THS, both prior to, and during, the COVID-19 pandemic. The DoH has also maintained a limited strategic reserve of pandemic PPE for surge capacity supplemented by the Australian Government National Medical Stockpile through prepositioned PPE in Tasmania. The COVID-19 pandemic has placed unprecedented pressure on supply chains worldwide, impacting on the availability of critical medical resources. This was particularly evident early in the pandemic (including in the lead up to the NWRH outbreak), where there was a rush to order a range of medical supplies including pharmaceutical and medical consumables, PPE and ventilators. Shortages were reported by known THS suppliers, particularly those sourcing stock from China. Alternative suppliers had to be identified and validated in a surging price market.
Further processes were established to monitor and manage stock in Tasmania centrally, complementing those implemented nationally. As an example, the DoH undertook a statewide stocktake of ventilators in March 2020. This led to the initial ordering of 80 ventilators from overseas as part of a strategy to triple existing ventilator capacity, with further orders made as appropriate ventilator stockers were identified and the bona fides of the vendor and distribution certainty validated. As at 30 July 2020, Tasmania has 188 ventilators, comprising 66 ICU standard ventilators, 48 transport ventilators and 74 anaesthetic ventilators, with 128 ventilators still to be delivered. It is expected the orders on the remaining ventilators will be completed later in 2020, which will bring the overall number of ventilators available in Tasmania to 316.
For pharmaceutical supplies, the DoH developed a range of strategies to ensure the THS was able to manage stock levels, including:
- A framework to identify medicines required for the management of COVID-19 patients across a variety of hospital settings (e.g. including those used in emergency departments, COVID-19 wards, ICU and in palliation).
- A strategic stock management plan with stock levels based on the expected percentage of infected patients requiring hospitalisation, the expected length of stay of a COVID-19 patient and the number of ICU beds available. Stock levels are monitored using a dashboard approach with the aim of maintaining a rolling buffer of stock.
- Viewing and analysing the manageable volume of elective surgery in this context, given the fact that both anaesthesia for both surgical patients and ventilated ICU patients often call on the same limited stock of medications.
Statewide availability of ventilators, medical consumables and pharmaceutical supplies was also monitored daily from 15 March 2020. This included information on available ICU beds, ventilators, negative pressure rooms, COVID-19 beds and Hospital in the Home beds across the RHH, LGH, NWRH and Mersey Community Hospital (MCH). This information assisted a senior executive PPE Lead within the DoH ECC to manage logistics and statewide supply of PPE, and the Executive Director, Statewide Hospital Pharmacy Operations, THS, to manage pharmaceutical supply.
Tasmania shares information on the availability of critical equipment and consumables with other jurisdictions via national forums including National Cabinet and AHPPC. This informs national decision‑making regarding management of essential resources to support the COVID-19 response. For example, jurisdictions agreed early in the pandemic to share information on ventilator numbers to support management of the National Medical Stockpile.
Tasmania has now created a State Emergency Management Stockpile of COVID-19 PPE, that will comprise six months of surge capacity PPE on top of standard PPE supplies. Further information in relation to PPE is contained in section 5.
1.8.1 Elective surgery restrictions
Another measure to help ensure the health system had appropriate capacity and resources (including beds and PPE) to respond to COVID-19 was the temporary suspension of all non-urgent elective surgery in both the public and private sector. This was announced by the Prime Minister on 25 March 2020 (acting on the advice of AHPPC). The Tasmanian Minister for Health announced on the same day that, in accordance with the Prime Minister’s decision, from 11:59PM that night, only category 1 and some exceptional category 2 surgery would continue.
The temporary suspension of non-urgent elective surgeries played a vital role in ensuring the Tasmanian health system’s capacity to respond to COVID-19 by ensuring facilities were available to accept any COVID-19 patients, and to ensure adequate supplies of PPE and other necessary supplies were maintained. The national restrictions on non-urgent elective surgeries continued through most of April.
On 21 April 2020, National Cabinet announced some non-urgent elective surgeries could commence from 27 April 2020, with the aim to restore 25 per cent of previously closed theatre capacity. The DoH worked closely with the THS and private hospitals in Tasmania to increase the availability of elective surgery from that date, while having regard to a set of National Principles, to ensure the increase in elective surgery activity did not adversely impact on PPE, pharmaceuticals, ventilators and levels of other stock that may be needed to treat COVID-19 patients.
The DoH took a cautious approach to increasing elective surgery activity given the North West outbreak, viewing the 25 per cent uplift as a ceiling rather than a target. This expectation was also communicated to private providers. The exact volume of elective surgery to be delivered in each hospital was dependent on their capacity and the measures they had in place to manage potential COVID-19 outbreaks. As a result, the initial uplift in elective surgery activity was initially confined to southern Tasmania.
From 27 April 2020 to 3 May 2020, there was no uplift in elective surgery in the north or north west, while the NWRH and NWPH were being recommissioned and the LGH was supporting the NWRH and NWPH during that time. Calvary Health Care facilities in Launceston also did not ease their restrictions on non-urgent elective surgery during that time due to their role in supporting the LGH. A limited amount of elective surgery activity commenced in North West Tasmania from the week of 4 May 2020.
The DoH has strong collaborative relationships with the private hospital sector in Tasmania and worked with private providers to sustain total hospital capacity prior to, and during, the outbreak. This was also aided by the implementation of financial viability payments for private hospital operators across Australia. On 31 March 2020, the Australian Government announced that in response to the temporary suspension of non-urgent elective surgery, it would guarantee the viability and capacity of the private healthcare sector. The DoH entered into agreements with a range of private healthcare operators in Tasmanian to formalise these guarantee arrangements. Under these agreements, private hospital operators were required to support the DoH’s response to the pandemic by providing certain services, including:
- providing clinical services;
- providing appropriate facilities, resources, supplies and other support services;
- making PPE, medical equipment, supplies and consumables available for a coordinated response by the DoH in meeting demand arising from the pandemic; and
- temporarily redeploying personnel and equipment at the direction of the DoH to assist its response to the pandemic.
Private operators had been providing COVID-19-related assistance to the THS well before the guarantee agreements were signed. The THS commenced discussions with private hospital operators in March 2020 regarding their ability to provide additional capacity if required. As a result, during the temporary closure of the NWRH, Calvary’s two Launceston facilities (St Vincent’s and St Luke’s) both accepted the LGH emergency theatre list, while St Luke’s also performed more urgent public patient orthopaedic surgeries, before finalisation of an agreement.
1.9 Health service restrictions
During March 2020, in addition to the temporary suspension of non-urgent elective surgery, other Tasmanian Government health services developed business continuity plans and management guidelines to limit their activities in order to preserve health system capacity and resources to prevent the further transmission of COVID-19, and maintain continuity for emergency or urgent cases in the event of an outbreak.
The plans were designed to allow health services to maintain delivery of essential services during any unplanned interruption to service delivery capability. They set out how each health service area would operate following disruption and how the service area would return to “business as usual’ as quickly as possible afterwards. This planning helped minimise disruption from unexpected events and provided staff with knowledge of their responsibilities following escalation triggers.
For example, on 28 March 2020, the DoH Secretary endorsed Oral Health Services Tasmania’s business continuity plan for the COVID-19 pandemic. This resulted in Oral Health Services Tasmania moving to its level 2 response. As a result, from 30 March 2020 Oral Health Services Tasmania restricted its services to emergency/urgent services only in Devonport, Burnie, New Town, Launceston, Clarence and Glenorchy, and fully closed its small community clinics.
Dental services require the use of significant quantities of PPE, due to the frequency of aerosol-generating procedures, as well as the close proximity of the dental team to the client when providing care. Restricting Oral Health Services Tasmania to provide only essential services was particularly important to conserve the use of PPE leading up to, and during, the outbreak, and to protect practitioners, patients and clients.
